Like many mental health conditions, obsessive-compulsive disorder (OCD) is often misunderstood. TV shows portray people with OCD as “quirky,” rigid, and inflexible. People who call themselves “neat freaks” may claim to have OCD. Cleanliness is one aspect of OCD, but it is much more complicated than that.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder (OCD) is a mental disorder in which you have uncontrollable reoccurring thoughts and behaviors. These are called obsessions and compulsions. If you have OCD, you may have obsessions, compulsions, or both. Obsessions cause anxiety, and performing compulsions reduces that anxiety.
Some people with OCD know their thoughts are unrealistic, but they can’t stop them. Others may believe their obsessive thoughts are true. They may feel like something terrible will happen if they don’t perform their rituals.
Common obsessions in people with OCD include:
- Fear of germs or contamination
- Disturbing sexual thoughts or images
- Religious, usually blasphemous, thoughts or fears
- Extreme concern with order and symmetry
- Fear of losing something important
- Fear of harming someone or being harmed
Common compulsions include:
- Excessive cleaning or hand washing
- Repeatedly checking on things, such as making sure the door is locked
- Ordering and arranging objects in a particular, precise way
- Constantly seeking approval or reassurance
- Compulsive counting or preferring/avoiding certain numbers
- Avoiding places, people, or situations that cause distress and trigger obsessions or compulsions
More than 2.5 million people in the United States live with OCD. Women are three times more likely to have OCD than men. It usually starts around age 19, although 25% of cases occur by age 14. A third of adults with OCD first experienced symptoms in childhood.
Are there different types of OCD?
There isn’t an official way to divide OCD into subtypes. However, research suggests there are four main categories:
- Cleaning and contamination: Contamination OCD involves a fear of bodily fluids, dirt, germs, and illnesses. With contamination OCD, you might doubt whether objects are really clean.
- Symmetry and ordering (“just right OCD”): A common theme of “just right OCD” is a feeling of incompleteness. You might feel intense discomfort if objects aren’t arranged properly.
- Forbidden, harmful, or taboo thoughts and impulses: This type of OCD usually involves unwanted obsessions around religion, sex, or violence. This can include having impulses to hurt someone, even though you aren’t a violent person.
- Hoarding: Hoarding OCD involves intrusive thoughts about acquiring possessions and having difficulty getting rid of them. It is separate from hoarding disorder, which involves holding onto items because you believe you need to save them.
These categories are also known as symptom dimensions. Some symptoms may be similar for many people with OCD, but others can vary significantly. It is also possible to have symptoms from more than one dimension.
What causes OCD?
Scientists don’t know exactly what causes OCD. But there are several theories around potential causes, including:
- Genetics: People with a first-degree relative with OCD have a higher risk of developing it. A first-degree relative is a parent, sibling, or child. The risk is higher if the relative developed OCD as a child or teen.
- Environment: Some studies have found an association between childhood trauma and OCD symptoms. Some children develop OCD symptoms after having a streptococcal infection, such as strep throat.
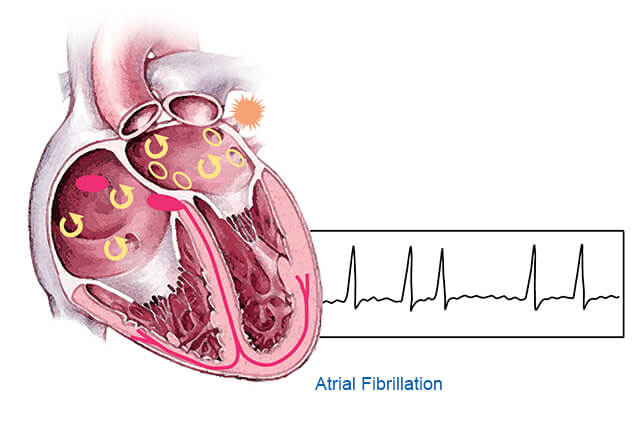
- Brain structure and functioning: There may be a connection between OCD symptoms and abnormalities in certain parts of the brain. The connection isn’t clear, and experts are still conducting research. However, imaging studies have shown differences in the frontal cortex and subcortical brain structures in people with OCD. Certain parts of the frontal cortex are responsible for judgment, self-control, emotions, and more. The subcortical region of the brain plays a role in cognitive and social functions.
How is OCD treated?
OCD is a lifelong condition, and currently, there is no cure. However, many people with OCD experience symptom improvement with treatment.
The first-line treatment for OCD is psychotherapy. Cognitive behavioral therapy (CBT) is one of the most common forms of psychotherapy. A type of CBT used to treat OCD is exposure and response prevention (ERP). Patients are exposed to feared situations or images that focus on their obsessions. They are told not to perform their compulsion. Exposing patients to a feared situation without something bad happening can help them understand their fearful thoughts are just that—thoughts. This helps patients learn to cope without their compulsions over time.
Medications like serotonin reuptake inhibitors (SSRIs) can help treat OCD symptoms. An SSRI increases the levels of serotonin in the brain. OCD is linked to low serotonin levels, but the connection isn’t clear.
A combination of medication and psychotherapy is usually the best treatment for OCD. If that doesn’t work, your doctor might try other treatment options:
- Deep brain stimulation involves implanting electrodes within certain parts of the brain. The electrodes produce electrical impulses that help regulate abnormal impulses.
- Transcranial magnetic stimulation uses magnetic fields to stimulate nerve cells in the brain. This helps improve OCD symptoms.
Living with OCD can be difficult, but treatment can help. If you have OCD, talk to your doctor about your treatment options.
Resource links:
"Obsessive-Compulsive Disorder" via MedlinePlus
"What is Obsessive-Compulsive Disorder?" via American Psychiatric Association
"Anxiety Disorders - Facts and Statistics" via Anxiety & Depression Association of America
"Obsessive-compulsive disorder and its related disorders: a reappraisal of obsessive-compulsive spectrum concepts" via Dialogues in Clinical Neuroscience
"Obsessive Compulsive Disorder" via National Institute of Mental Health
"Obsessive-compulsive disorder (OCD)" via Mayo Clinic