As a patient, you want to be educated about your condition and treatment options. The best way to do this is by asking your oncologist questions.
It's also important to ask for clarification during appointments, especially when doctors use medical words or explain complex topics. Bring a notebook or tape recorder to your appointment, so you can write down the answers or record an audio recording.
1. What is immunotherapy?
Immunotherapy is a type of cancer treatment that uses your immune system to prevent, control, or eliminate cancer. It can be used alone or in combination with surgery, chemotherapy, or radiation therapy.
Some immunotherapy treatments work by targeting specific proteins on cancer cells, called antigens. These drugs are known as checkpoint inhibitors and include rituximab (Rituxan) and pembrolizumab (Keytruda).
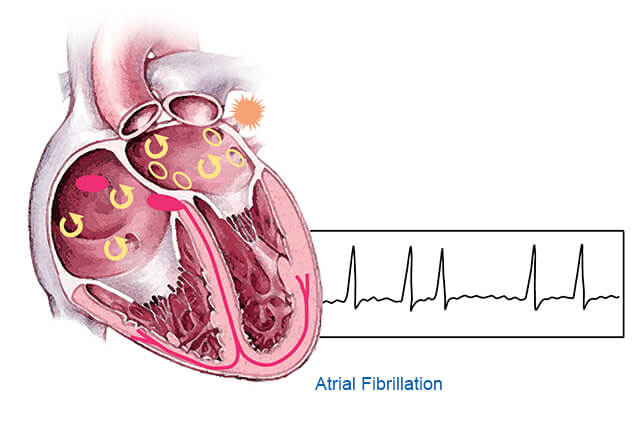
Other immunotherapy treatments boost the ability of T lymphocytes, or T-cells, to fight cancer by adding receptors that make them better able to recognise and destroy tumour cells. Examples of these treatments include chimeric antigen receptor T-cell therapy, and tumor infiltrating lymphocyte, or TIL, therapy. Some types of immunotherapy rev up your immune system and can cause side effects, such as fever, chills, fatigue, a runny nose, weight gain from extra fluids, heart palpitations, or vomiting.
2. What are the side effects of immunotherapy?
Immunotherapy drugs help your immune system fight cancer by tinkering with it. But just like any treatment, immunotherapy can have side effects that may impact various organs and body systems.
Some of these are mild, others can be severe or even life-threatening. Any new or worsening health problems should be reported to the team immediately, as it is easier to treat early.
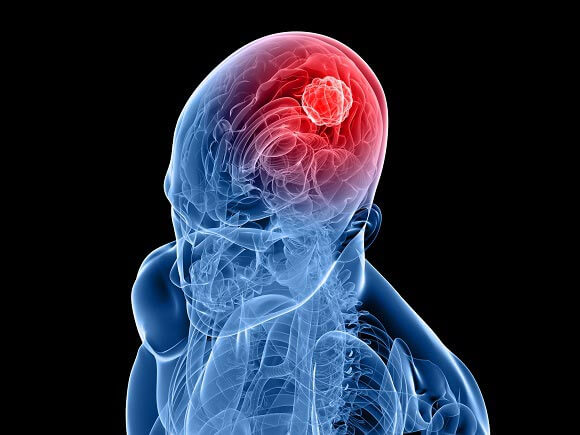
The most common side effects of immunotherapy are fatigue and anything that ends with -itis (colitis, inflammation of the lungs)—this isn’t surprising since immunotherapy drugs tinker with your immune system. Other symptoms include a fever, chills or rashes, headache, indigestion and trouble breathing. Some of these side effects can be treated with medication. Others can’t, and in some cases the side effects can linger after the medicine is out of your system.
3. What are the goals of immunotherapy?
Immunotherapy aims to use your own body’s natural defense systems to find and destroy cancer cells. It can be effective when other treatments aren’t. It can also help your immune system “memorize” cancer cells so they’re less likely to return (immunomemory).
Your immune system consists of white blood cells and the organs and tissues of your lymph system, like your thymus, spleen, lymph nodes, and bone marrow. Immunotherapy drugs make your immune system work harder or better, so it can more easily find and get rid of cancer cells.
Other immunotherapy options include adoptive cell therapy, which takes your own immune system cells and enhances or modifies them in a lab, so they can better find and attack cancer cells; and oncolytic virus therapy, which uses a genetically modified virus to kill cancer cells.
4. What are the risks of immunotherapy?
Most immunotherapy causes side effects, but they are usually less severe than those associated with other cancer treatments. You should tell your health care team about any new or worsening symptoms, even if you think they are not related to treatment. They will want to know about them so that they can help you feel better as quickly as possible.
Some immunotherapies cause problems in the bone marrow, where blood cells are made. This can lead to too few red blood cells (anemia), too few platelets (thrombocytopenia) or low white blood cell counts (neutropenia).
These medications cause the immune system to become overactive, leading to inflammation in various parts of the body. This is called an immune-related adverse event, or irAE. This risk is higher if you take more than one of these drugs at the same time or have a history of autoimmune disease.
5. What are my options for immunotherapy?
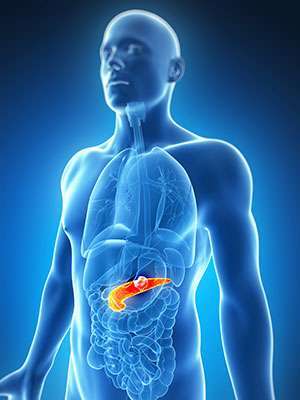
The type of immunotherapy you receive depends on the location and stage of your cancer, its response to previous treatments and biomarkers identified by tumor testing. FDA-approved immunotherapies include targeted antibodies and checkpoint inhibitors.
Ask your doctor to describe the goals of each therapy, how it will help you and the potential side effects. Remember to ask about other options for managing side effects, such as nutrition and dietary supplements, physical therapy, naturopathic support and psychiatry.
If you are worried about remembering all of your questions during the appointment, write them down ahead of time or bring a notebook to record your conversation. It can also be helpful to have a friend or family member with you for emotional and practical support.